|
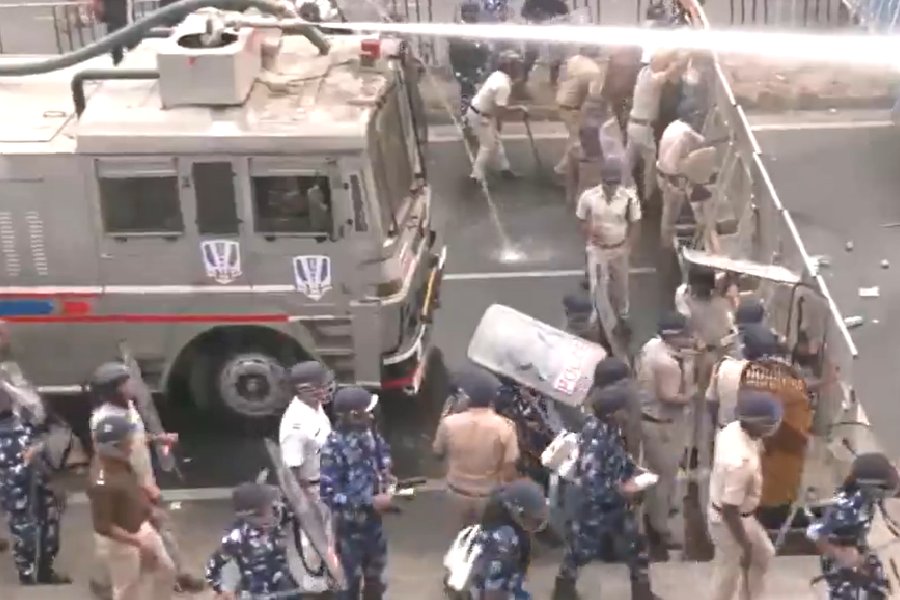
| Nurse coordinator Lisa Chrisley (left) injects an experimental vaccine into volunteer Michelle Levender, a medical school student, during a clinical trial to test the effectiveness of the vaccine to combat avian influenza at the University of Maryland School of Medicine in Baltimore, Maryland, in April this year. (File picture) |
Hyderabad, Oct. 23: Neither government regulators nor ethics watchdogs in India have adequately equipped themselves to protect the interests of patients who volunteer for clinical trials of new and unproven treatment, clinical research experts have said.
While top government officials have announced plans to register and inspect clinical trials in India, experts warned that gaps in the skills of researchers and ethics committees have created the potential for exploitation of vulnerable sections of patients.
“While deliberate malpractice might be rare, the system is ripe for errors to fall through huge cracks,” Falguni Sen, professor at Fordham University in New York said at a two-day conference here, called to find ways to improve India’s capacity for clinical trials.
The low cost of research and ease of finding large numbers of patients with different illnesses have made India an attractive site for trials. The industry estimates that India earned $70 million last year from clinical trials and could aim at $1 billion revenues within the next five years.
But several unapproved, illegal clinical trials have taken place in different cities over the past five years ? some of them involving drugs or technologies developed in foreign countries ? giving rise to concerns that Indian patients have been used as “guinea pigs” for experimental therapies.
Amid such concerns, the debate on how India should prepare for clinical trials has intensified. Proponents have argued that clinical trials would benefit India by helping build expertise for good clinical practice. “The biggest gain would be an improvement in quality of medical services provided by doctors,” said Dhananjay Bakhle, a senior drug industry official.
Clinical trials demand that doctors follow good clinical practices and they will learn and apply them on other patients, he said.
Indian drug regulators estimate that about 100 clinical trials of drugs developed outside India are currently under evaluation in the country. “The minute India is added to global multicentric trials, the number of patients rises really fast,” said Bakhle.
But conference presentations indicated that India is ill-prepared to handle burgeoning trials. “Even on paper, only 40 out of 179 ethical committees that are supposed to approve and monitor trials in medical colleges and research institutes today meet prescribed guidelines,” said Vasantha Muthuswamy, deputy director general in the Indian Council of Medical Research.
Independent studies have also revealed gaps in skills of medical researchers and institutions that might line up to participate in trials. “Few investigators have experience in conducting large-scale disease studies which would have automatically prepared them for clinical trials,” said Sen.
Sen’s investigation of clinical trials in India has also shown that specialised testing equipment for trials is often unavailable in locations where trials could otherwise be conducted. “A number of hospitals look at trials as a way of getting state-of-the-art equipment from drug companies and are also interested in enrolling as many patients as possible,” he said.
Experts at the two-day workshop, organised by Fordham University and the Indian Council of Medical Research at the Administrative Staff College of India, said India might need to set up new mechanisms to protect the interests of people who are subjected to experiments.
“The regulatory and legal system in India is not equipped to take care of negligence in this area,” Sen said. The US has an Office of Human Research Protection, specially created to protect the interests of patients involved in medical experimentation.
Muthuswamy said legislation that would make ethical practices binding on all researchers and institutions involved in clinical trials has been approved by the government and is expected to be introduced in Parliament soon. “We’ve specified penalties for violations of ethics,” she said.
Government officials at the conference said clinical trials would be registered and audited. “We plan to inspect 20 clinical trials per year to ensure that they comply with good clinical practice,” said Ashwini Kumar, drugs controller of India.
Patients with heart disease and cancer are among victims of illegal clinical trials that have been conducted in the country over the past decade.