|
 |
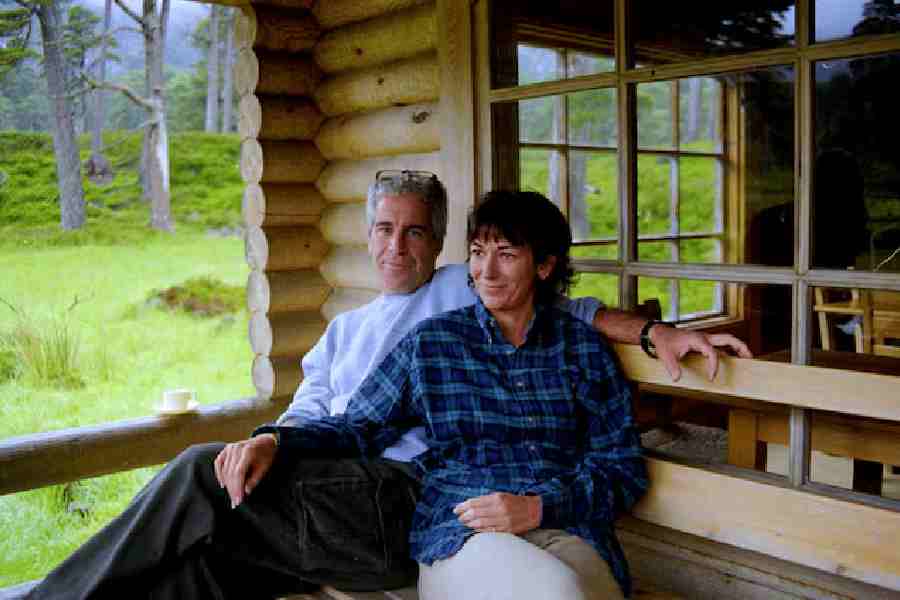
| LIFELINE: Thalassaemic children receiving blood transfusion at Samarpan Blood Bank, Mumbai. Pic: Gajanan Dudhalkar |
Bharati Jadhav is the quintessential bride — madly in love and planning a rosy future with her husband. In one respect, however, she is not like other newlyweds. The 22-year-old clerk at the Brihanmumbai Municipal Corporation has decided she is never going to have a child.
That’s because Bharati is a thalassaemia major, or a person who has the disease, as opposed to thalassaemia minors, who only carry and pass on the defective gene. India has some one lakh thalassaemia majors. Forty million Indians, including Amitabh Bachchan, are thalassaemia minor.
Bharati knows she is lucky to be weaving dreams with her husband even as she goes for regular blood transfusions and removal of extra iron from her blood. “I don’t worry about death — even healthy people die of accidents. It’s important to live,” she says.
Different strains of thalassaemia exist. They are a group of hereditary blood disorders that share one feature — the defective production of haemoglobin, the protein required to help red blood cells carry oxygen.
In India every year, over 10,000 children are born with thalassaemia. Only 5-10 per cent receive the right kind of treatment and most do not live to see 20.
But in recent times better treatment and easier medication have made it possible for many patients to live longer. There was a time when majors needed to inject themselves with an iron chelator to remove excess iron from their blood, which is one of the side-effects of transfusion and can be fatal. But now oral drugs, though expensive, are available.
Health experts point out that in many parts of the world, thalassaemia has been controlled and majors have been encouraged to lead normal lives. In Cyprus, for instance, 38 per cent of thalassaemic majors are married and have children.
The issue came up at a recent workshop on managing thalassaemia in Mumbai. “We were surprised to find a couple of thalassaemia major girls who had got married to healthy youngsters,” says Vinay Shetty, a member of Think Foundation which deals with thalassaemia and had convened the seminar along with the paediatric wing of the Lokmanya Tilak Municipal General Hospital.
Genes responsible for thalassaemia are relatively common in places where malaria was endemic. Being a thalassaemia minor afforded protection against malaria, and the gene thrived.
In India, Bengalis, Sindhis, Punjabis, Gujaratis (especially Lohanas and Kutchis) and some tribal and Muslim groups are high risk communities. According to the Indian Council of Medical Research, nine out of 100 people in Calcutta are affected by thalassaemia — as compared to two or less in Delhi, Mumbai, Chennai and Bangalore. About 10 per cent of all thalassaemia cases are in Bengal. Thalassaemic majors have to go through lifelong transfusions, once in two or four weeks, which cost around Rs 2,000-2,500 a month.
But Bengal is one of the few Indian states, along with Gujarat, which has been trying to tackle thalassaemia. Calcutta’s Thalassaemia Association is active in creating awareness and has found a champion for their cause in actor Mithun Chakraborty, who is also a blood donor. Blood donation drives are organised and thalassaemic centres have been established in all hospitals in Calcutta. The situation outside the capital, however, is still poor.
“The state government has realised that even if we do massive awareness campaigns there are no facilities for diagnosis in rural areas or smaller cities,” says Dr Sharmila Chandra, a haematologist who also has a blood bank which she runs with the Lions Club and her non governmental organisation Jana Chetana Foundation. “So we need to lay stress on prevention. We spend Rs 40,000 or more on a marriage, but why can’t we spend Rs 300 on a thalassaemia test for our peace of mind?”
Many believe that if people know they are thalassaemic, the number of thalassaemic babies can be controlled. A thalassaemic major’s child will always carry the genetic disorder. There is a 25 per cent chance that the child of two thalassaemic minors will be a major.
A certificate before marriage, some argue, can tackle thalassaemia. Many experts also believe that it should be mandatory for a doctor to do a thalassaemia test on a pregnant woman. People working with thalassaemia believe that gynaecologists should recommend thalassaemia tests to prevent the birth of thalassaemic babies.
If the gynaecologist treating Mumbaikar Parth Dalal’s wife had insisted on a test in the first term of her pregnancy, they wouldn’t have lost their two-year-old child. For his second child, he went for a pre-natal test and found that the son was free of the defective gene. Now, they are actively helping in thalassaemia awareness. “We need to match thalassaemia reports, not kundlis,” his wife says.
Not all parents are like the Dalals. The parents of Sana, an eight-year-old girl who comes with her mother for blood transfusion every fortnight to the Samarpan Blood Bank in Ghatkopar in Mumbai, knew they were Thalassaemia minors and that Sana was a major. Yet, they kept trying for a baby boy. A boy was finally born — and turned out to be a thalassaemia major.
“You give people advice but they don’t necessarily take it,” rues Zahida Khan, a nurse at Samarpan. Khan, who recently lost her 15-year-old daughter, left her husband when he suggested they dump their ailing child.
Taking care of a thalassaemic child is difficult. Darshana, who works with the Samarpan Blood Bank in Mumbai, has a 15-year old thalassaemia major son, Smit. She ensures that he eats cheese and paneer regularly, since calcium is good for the bones which become brittle because of the high iron in the blood. She avoids iron-rich food such as beetroots, carrots, green leafy vegetables and beans. A careful diet and medication enables her son to lead a normal life — he even went to Kullu and Manali from school recently.
Those working with thalassaemic children hope the government will do more for prevention. In countries where thalassaemia is endemic, governments have intervened to work on prevention — and succeeded. Cyprus, where pre-marital screening was made compulsory, started pre-natal diagnosis in 1984. No thalassaemic babies have been born in the last five years. Most patients are over 25 years old.
In India, Gujarat — which has 3,000 thalassaemia patients — has taken a few proactive steps. In Rajkot, students at a women’s college are required to undergo a thalassaemia test before they can receive university mark sheets. Among the Lohana and the Kutchis, it is a given to ask for thalassaemia status reports in an arranged marriage. The downside, of course, is that non-thalassaemic people often call off matches when they find that their would-be partner is thalassaemic.
Experts say that the government needs to initiate a national prevention programme for thalassaemia. “Unlike many other genetic disorders, when carriers cannot be easily identified, the thalassaemiacs give us enormous opportunity to implement effective national screening programmes to control affected births by community information, screening, counselling and pre-natal diagnosis,” says the Indian Journal of Human Genetics in a 2010 issue. “The only solution for India is to implement a national screening programme immediately, but this can only be successful if there is political will.”