Devi Shetty’s Narayana Health has launched its health insurance products in Calcutta, promising to eliminate the mistrust between insurers, hospitals and patients while reducing lengthy wait times for claim settlements after discharge.
The Bengaluru-based healthcare chain, which runs three hospitals in Calcutta and its neighbourhood, has introduced two insurance products through its new venture, Narayana Health Insurance Ltd (NHIL): Aditi and Aditi Plus, which were first launched in Bengaluru and Mysuru last year.
Aditi offers comprehensive coverage with ₹1 crore for surgical procedures and ₹5 lakh for medical treatment annually, for a premium of ₹12,000 per year for a family of four. Customers receive treatment in general hospital beds.
Aditi Plus provides coverage of ₹1 crore for surgeries and ₹20 lakh for medical treatment annually at ₹29,000 per year, with access to private rooms during treatment.
Premiums may vary based on age and clinical criteria, NHIL officials noted.
The insurance scheme directly tackles two major complaints patients have against hospitals and insurance companies: incomplete reimbursement despite claims falling within policy limits, and extended waiting periods after doctors advise discharge.
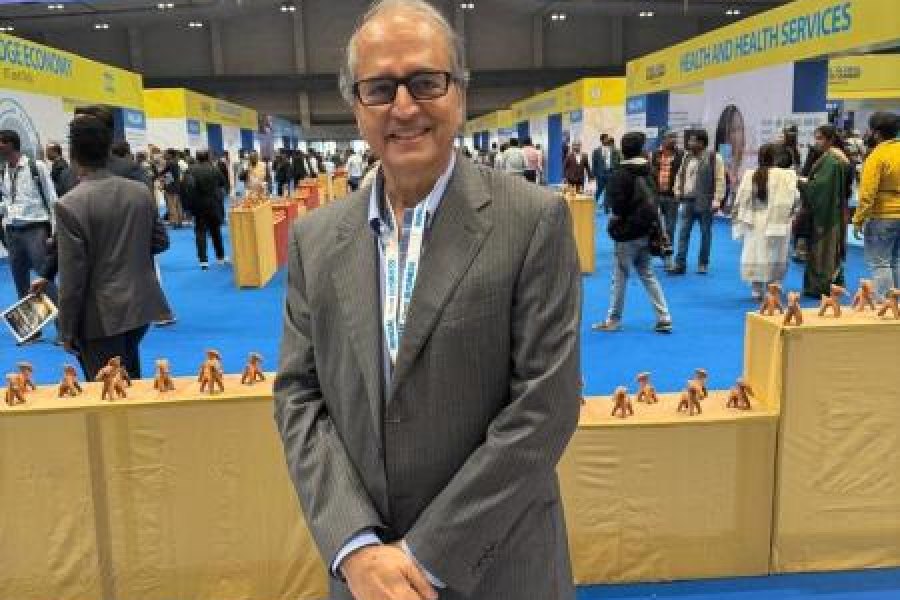
“The policy will cover non-medical expenses, and there should not be a waiting period for patients after discharge,” said Ravi Vishwanath, director of NHIL.
He said the root cause of these problems is the lack of trust among hospitals, insurance companies and patients. “In this case, the mistrust issue will be removed since the insurance company and hospital are owned by the same healthcare group.”
While the insurance policy is primarily designed for Narayana Health’s network of approximately 20 hospitals across India, customers can seek treatment at other facilities when necessary.
“If the treatment is not available at NH hospitals or in cities where the group doesn’t have presence, we will request cashless facilities from other hospitals. If rejected, we will reimburse the consumer post-hospitalisation,” Vishwanath said.
The scheme targets India’s “missing middle” – an estimated 100 million people who have some disposable income but lack coverage under government insurance schemes, according to Narayana founder Devi Shetty.
“The scheme is aimed at removing inequality in healthcare access for people who cannot afford quality treatment because of affordability issues,” Shetty had said after the initial launch last year.
R. Venkatesh, group COO of Narayana Health, emphasised the unique positioning: “Built on our core belief in delivering passionate care to patients, this initiative allows families to choose the
same trusted name for both care and coverage, which is also a first for India.”
A government health insurance company official acknowledged the potential of such schemes but highlighted a crucial limitation: effectiveness depends on having an extensive hospital network nationwide.
“The moment patients go to hospitals which are not under the healthcare group that is also the insurer, then the trust issue will crop up, along with the usual problems of delay and partial reimbursement on the pretext of not following treatment protocols,” the official warned.
The success of Narayana Health’s integrated model could influence how other healthcare chains approach insurance, potentially reshaping India’s healthcare industry structure.