What exactly is a sexually transmitted infection (STI)? Is it the same as an STD? How can I recognise the symptoms of an STI? Would it be really bad if I got one?
If you are a ’90s kid in Kolkata, you probably grew up somewhat confused (or somewhat amused) by the Buladi campaign ads where a doll in a sari urged people to wear condoms during the height of the global HIV/AIDS epidemic.
HIV/AIDS was a deadly sexually transmitted infection (STI) till the early 2000s, and thanks to global efforts around condom-use and awareness, we have come a long way since. HIV/AIDS is now much less rampant in our country, we have options for prevention (like PrEP) for high-risk populations, and it can be treated to become undetectable (and also untransmittable).
Unfortunately, we have not maintained the same fervour around public health education for STIs other than HIV/AIDS, despite how common they are.
Sexually transmitted infections (STIs) are infections that are transferred mainly through sexual contact, such as HIV, chlamydia, syphilis, HPV and herpes. These used to be called sexually transmitted diseases (STDs), but the newer name is supposed to reflect that STIs don’t always develop into symptomatic diseases. STIs can be caused by bacteria, parasites or viruses, and can be transmitted mainly via oral, vaginal or anal sex.
‘No symptom’ is the most common symptom
Remember when people were infected with COVID19 and could be asymptomatic carriers without even realising it? STIs can do a similar thing, and the most common “symptom” of an STI is that there are no symptoms at all. The WHO estimates that globally over 1 million people acquire an STI every day, most of which are asymptomatic.
If STIs being this common is new information to you, it is okay to feel a little worried. However, it is important to note that many STIs are in fact curable (such as chlamydia, gonorrhoea, syphilis). Some still can’t be cured (such as herpes simplex virus (HSV), human papillomavirus (HPV) or hepatitis B). However, for all of them, you can manage the symptoms through early detection and treatment. A large part of the stress around STIs, unsurprisingly, comes from the social stigma around them — and the fact that most people don’t know a lot about them (think: early days of COVID while we were still figuring out what to expect).
You can ‘mask up’
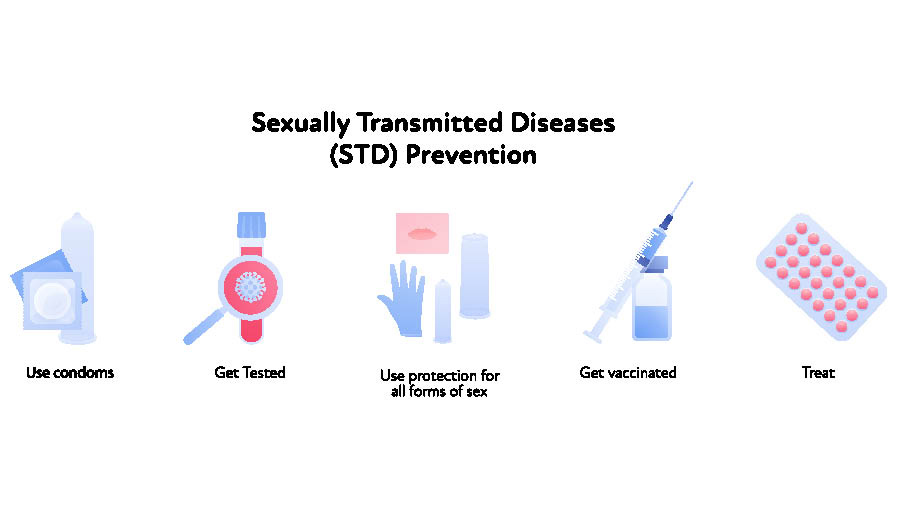
Just like with COVID-19, some people are more comfortable with STI risk than others. Condoms can help you ‘mask up’ against most infections. Barrier methods are your friend when it comes to STI transmission.
Condoms can be your friend in more than just preventing pregnancy — external or internal condoms can be used to reduce STI risk in vaginal sex, anal sex, oral sex to a penis (this is why they come flavoured!) or sex where you are sharing sex toys/dildos.
For oral sex with a vulva (outer part of the vagina) or anus, you can consider using a dental dam. The awkward name of these come from a small latex sheet used in dental procedures, but you can make them yourself at home by cutting open a condom and simply holding it outstretched in front of the vulva/anus.
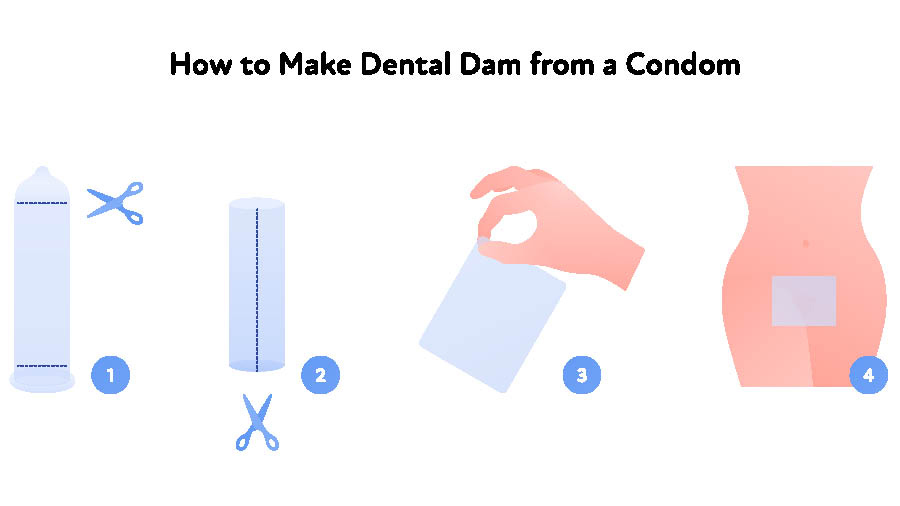
For oral sex with a vulva (outer part of the vagina) or anus, you can consider using a dental dam Shutterstock
Not a lot can be transmitted through kissing alone, but herpes simplex virus (HSV) can move through saliva if one of the partners has an active herpes sore. Often called ‘cold sores’, these are small sores around the mouth that people don’t even always associate with STIs — these are often even passed from parents/adults to children through non-sexual contact.
Stay ahead of the game by testing
At the peak of the pandemic, you may remember having to take COVID-19 tests before taking a flight or travelling somewhere new, even when you didn’t have any symptoms. In the same way, doctors recommend testing for STIs proactively through blood tests, swabs and pap-smears (depending on which tests you get) even if you don’t have symptoms. STI testing panels can be of varied levels of complexity, depending on what your level of risk is. For example, if someone tends to have multiple partners, or tends to have anal intercourse more often, they may need a more complex panel.
Testing can also become important if you display any symptoms of an STI. These could be new sores, bumps, rashes, warts, or unusual colour, smell or quantity of discharge (from a vagina) or any unusual discharge from a penis, repeated pain or bleeding during intercourse. This list is not exhaustive, because I encourage you to (a) test regardless of whether you have symptoms and (b) consult a doctor as soon as possible, if you do have symptoms.

The HPV (human papillomavirus) vaccine is an important one everyone should consider getting Shutterstock
Take some shots
Vaccines never hurt (metaphorically at least), and there is one important one everyone needs to get – the HPV (human papillomavirus) vaccine. It is also known as the ‘cervical cancer vaccine’ because when HPV (an STI) is left untreated it can develop into cervical cancer. This is a relatively newer vaccine, so if you are an adult today, it’s possible this was not part of your usual childhood vaccine protocol. Most cis girls are getting the HPV vaccine by age 9 now, and if you haven’t gotten it yet, you should head to your gynaecologist to get one ASAP. In India, it is currently only required for people with vulvas/vaginas, but in other countries it is also being administered to people with penises to reduce their risk of HPV (and potential penile cancer).
The only preventative drug for STIs is one for HIV named PrEP (pre-exposure prophylaxis). It can reduce risk of HIV by 99 per cent and is recommended by NACO for those who may be considered as ‘high risk populations’, for example people with penises engaging in anal intercourse, those who inject drugs, those who have a partner who has HIV, sex workers, etc.
Shutterstock
Take a breath and take stock
You don’t need to remember every scientific term, possible symptom and prevention method for every type of STI. Instead, just remember this:
- Get tested proactively and frequently
- Check in with your doctor if you feel something is awry with your body or feels off during intercourse
- Have open conversations with your partner(s) about whether they have been tested recently and/or if they have any symptoms. It can be a difficult conversation to have, but it is an important one! Perhaps your next date is to a testing centre.
- STIs are not shameful, they are super common and can be managed (if not cured)
Remember, you got this!
Karishma Swarup is a Kolkata-born and raised sexuality educator, Instagrammer (@talkyounevergot) and works at a global consulting firm. She busts myths about sex, pleasure, intimacy, orgasms, periods, and all things related to sexual health.
If you have a question you would like Karishma to answer, send an email on mykolkata@telegraphindia.com with the subject line ‘Questions for Karishma’ or DM/comment on our Facebook, Instagram, or Twitter.


