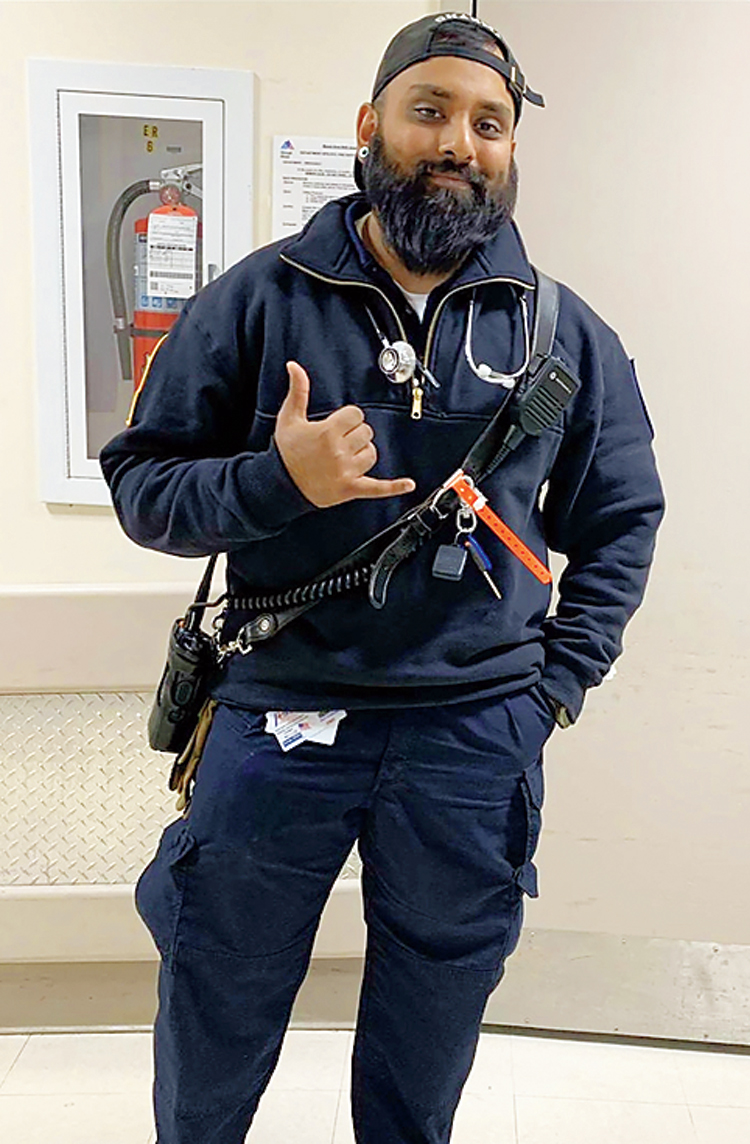
Ravi Sharma was doubled over on his bed when his father found him. He’d had a bad cough for a week and had self-quarantined in his bedroom. As an emergency medical technician, he knew he was probably infected with the coronavirus.
Now, Sharma, 27, could not move the right side of his body, and could only grunt in his father’s direction. His sister, Bina Yamin, on the phone from her home in Fort Wayne, Indiana, could hear the sounds.
“Call 911,” she told her father. “I think Ravi’s having a stroke.” She was right.
Over the next few hours, doctors at a Queens hospital worked frantically to break up a blood clot blocking an artery to Sharma’s brain. But the doctors were puzzled.
Sharma was far too young for a stroke. He worked out every day and didn’t have diabetes, high blood pressure or the kinds of medical conditions that can set the stage for strokes in young adults, which are rare.
Neurologists in New York City, Detroit, New Jersey and other parts of the country have reported a flurry of such cases. Many are now convinced that unexplained strokes represent yet another insidious manifestation of Covid-19, the illness caused by the new coronavirus.
The cases add to evidence that the coronavirus attacks not just the lungs, but also the kidneys, brain, heart and liver. In rare cases, it seems to trigger a life-threatening inflammatory syndrome in children.
“We’re seeing a startling number of young people who had a minor cough, or no recollection of viral symptoms at all, and they’re self-isolating at home like they’re supposed to — and they have a sudden stroke,” said Dr Adam Dmytriw, a University of Toronto radiologist who is a co-author of a paper describing patients who suffered strokes related to Covid-19. The paper has not yet been peer reviewed.
Though many of those patients had diabetes and hypertension, none had heart risks known to increase the odds of a stroke. Many were under age 65. For some, stroke was the first symptom of coronavirus infection, and they postponed going to the emergency room, fearing exposure.
Of 10 patients described in Dr Dmytriw’s paper, two died because the coronavirus attacked their lungs, and two men — a 46-year-old and a 55-year-old — were killed by strokes.
Doctors at Mount Sinai Health System in New York have also seen an unusual number of young stroke patients, saying they treated five such patients with Covid-19 during a recent two-week period. The medical centre typically sees only one stroke patient under the age of 50 every three weeks, Dr Johanna Fifi, a neurologist, and her colleagues noted in a letter in The New England Journal of Medicine.
Four of the five patients were relatively healthy; two patients in their 30s had no known risk factors for stroke. “We came to the conclusion it had to be related to Covid-19,” Dr Fifi said in an interview.
Though strokes seem to affect a very small number of Covid-19 patients, they appear to be related to a broader phenomenon that has emerged in critically ill patients: excessive blood clotting.
Patients with severe Covid-19 may develop clots in the legs and lungs that can be life-threatening, doctors said. Their blood can be so thick and viscous that it blocks intravenous lines and catheters. Tiny clots in other organs, like the kidneys and liver, have been found in autopsies of coronavirus patients.
Dr Michael Yaffe, an intensive care physician at Beth Israel Deaconess Medical Center in Boston, called clotting a “hallmark” of the disease, although “not in everyone”.
German scientists reported last week that autopsies of 12 Covid-19 patients turned up a type of blood clot called deep vein thrombosis in seven of them.
The cause of death in four patients was another type of blood clot in the lungs, called a pulmonary embolism.
Clotting is a risk in all critically ill patients if they are immobile for long periods. But patients with the coronavirus have elevated levels of clotting proteins in the blood, and the condition seems to be less responsive to blood-thinning drugs, said Dr Adam Cuker, an associate professor of medicine at the University of Pennsylvania.
Some evidence suggests that the coronavirus may directly infect the endothelial cells that line the inside of blood vessels, causing injury and swelling that draws proteins that promote clotting, Dr Cuker said.
People who have been exposed to the coronavirus, or are managing the infection at home, should call their doctors if they notice chest pain and shortness of breath, which may signal a blood clot in the lung, or leg pain, swelling, redness and discoloration that may indicate a clot.
Until he arrived at Jamaica Hospital on April 1, Sharma had never been tested for infection with the coronavirus. But he knew he was at risk.
He had spent weeks making back-to-back ambulance runs, ferrying sick, elderly patients from nursing homes to hospitals in Brooklyn and Queens in February and March.
By mid-March, Sharma had developed a dry cough. He went to an urgent care clinic, where he was told that it was out of tests, but that he should stay home because he was probably infected.
At the hospital, emergency room doctors took aggressive steps to restore the blood supply to the left side of his brain. They also diagnosed acute respiratory distress syndrome, finding that Sharma’s infected lungs were filling with fluid and his blood oxygen levels were low. A test revealed infection with the coronavirus, and he was placed on a ventilator.
The doctors were kind but honest with the family, Yamin said: “They told us that it was 50-50. They didn’t know if he would live or die.”
Over the next few days, while Sharma remained sedated, Yamin spoke frequently with the doctors and nurses at the hospital, taking meticulous notes that she shared with relatives and with The New York Times. New York Times News Service