Saturday, 27 April 2024
Saturday, 27 April 2024
 Saturday, 27 April 2024
Saturday, 27 April 2024









Art is a profound reality check. In creating an art object, the artist invites all of us to experience life without being attached to our conditioned understandings
T.M. KRISHNA

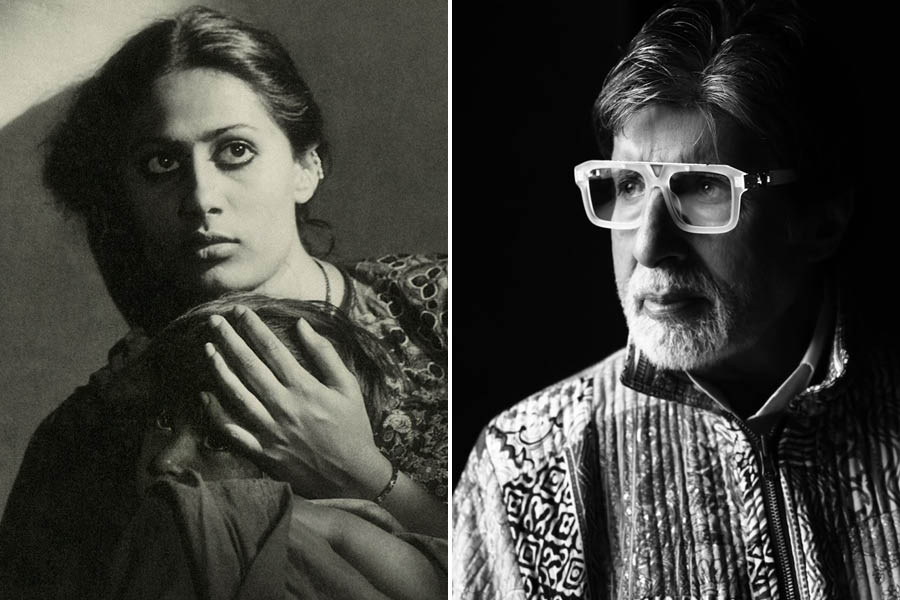
Bengali does not have one ‘single’ word for them, although they are variously described as unmarried, widowed, separated or divorced. Nor does Hindi. Not that they need new descriptions
CHANDRIMA S. BHATTACHARYA
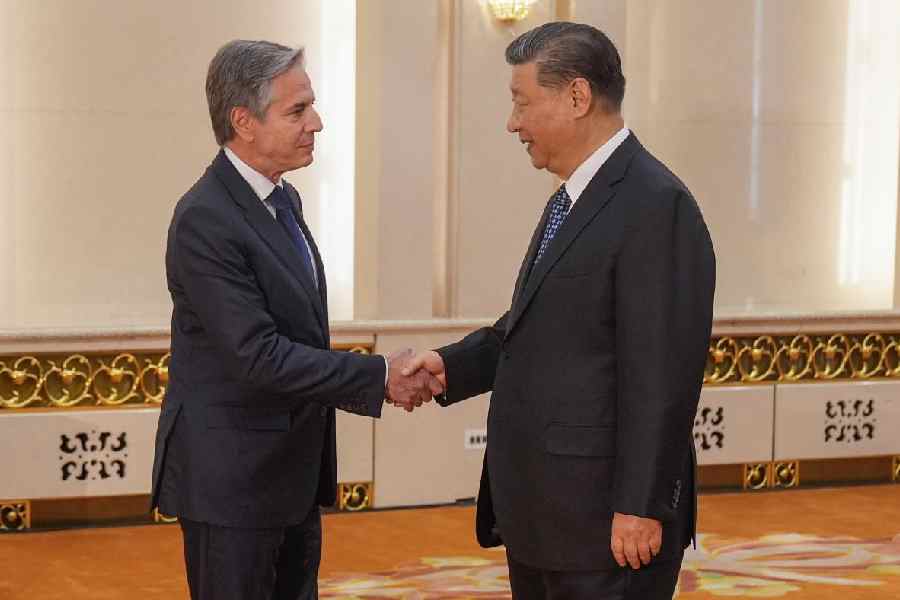
For the man who plays minder to Rahul Gandhi on his overseas visits, the Western media coverage seemed to imply that Modi had lost the plot and was on the cusp of being perceived as a global pariah
SWAPAN DASGUPTA
The fact that ‘working’ is as fluid a concept as gender needs to be focused in policymaking. This is because ‘work’ cannot be segregated in binary terms — private/public
SANHITA CHATTERJEE
Weaponisation of falsehood, malicious use of deflection to thwart reflection, contamination of truth — each of these elements is in play in elections in India & around the world
THE EDITORIAL BOARD































The film stars Paul Rudd, Carie Coon, McKenna Grace, Finn Wolfhard, Kumail Nanjiani, Dan Akroyd, Ernie Hudson and Bill Murray