Thursday, 09 May 2024
Thursday, 09 May 2024
 Thursday, 09 May 2024
Thursday, 09 May 2024















Planning a Turkish holiday? Anupam Roy has travel vignettes to share
Have you seen this Korean performance of ‘Phule Phule Dhole Dhole’?
Biryani on your mind? Head to Club Verde for a sumptuous Biryani festival
The trailer of ‘A Part of You’ promises to make you ponder over life and death
Try your hand at floral painting at ‘Brush and Bloom’ at The Bhawanipur House
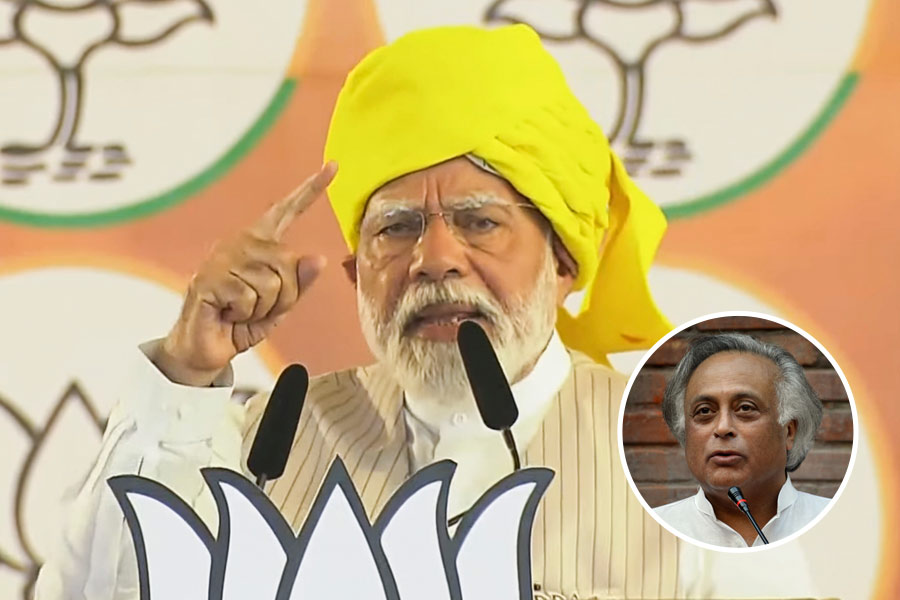
Intervening on social media, a chronicler of contemporary India recently complained that 'In fifty years of observing Indian elections I have never seen such vile and hate-filled rhetoric'
SWAPAN DASGUPTA

Travel writing was historically a lowbrow genre, both in terms of financial success & academic respectability, until two books appeared. One by Paul Theroux & the other by Paul Fussell
ABHISHEK CHATTERJEE
The current attempt by the American Right, therefore, is to change the nature of universities so that speaking the truth no longer remains their avowed objective
PRABHAT PATNAIK
Science should be rational and unaffected by political interests. Scientists should work with integrity and shouldn’t distort scientific results to please the political elite
BIJU DHARMAPALAN
Apart from projecting Vemula’s reasons for suicide as ‘personal’, report says Vemula never expressed any discontent with the university, ignoring his sarcastic letter to the VC
THE EDITORIAL BOARD
































From comedy to fantasy, dive into these movies if you are craving more of Hathaway after watching The Idea of You on Prime Video